Is Leg Swelling Serious? Signs Your Edema Is a Vascular Issue
Leg swelling is a common complaint that many people experience at some point in their lives. Often, it is a minor annoyance caused by standing for too long or a long flight. However, persistent or severe swelling can be a warning sign of an underlying health issue. Understanding leg swelling causes is the first step toward protecting your long-term health.
While fluid retention in the legs can stem from various factors, vascular conditions remain a primary culprit. Ignoring vascular swelling symptoms can lead to complications, including skin ulcers or blood clots. Recognizing the swollen legs meaning in the context of vein health allows for early intervention and effective management. This guide explores how to distinguish general swelling from vascular conditions and why seeking professional care is essential.
What Is Leg Swelling?
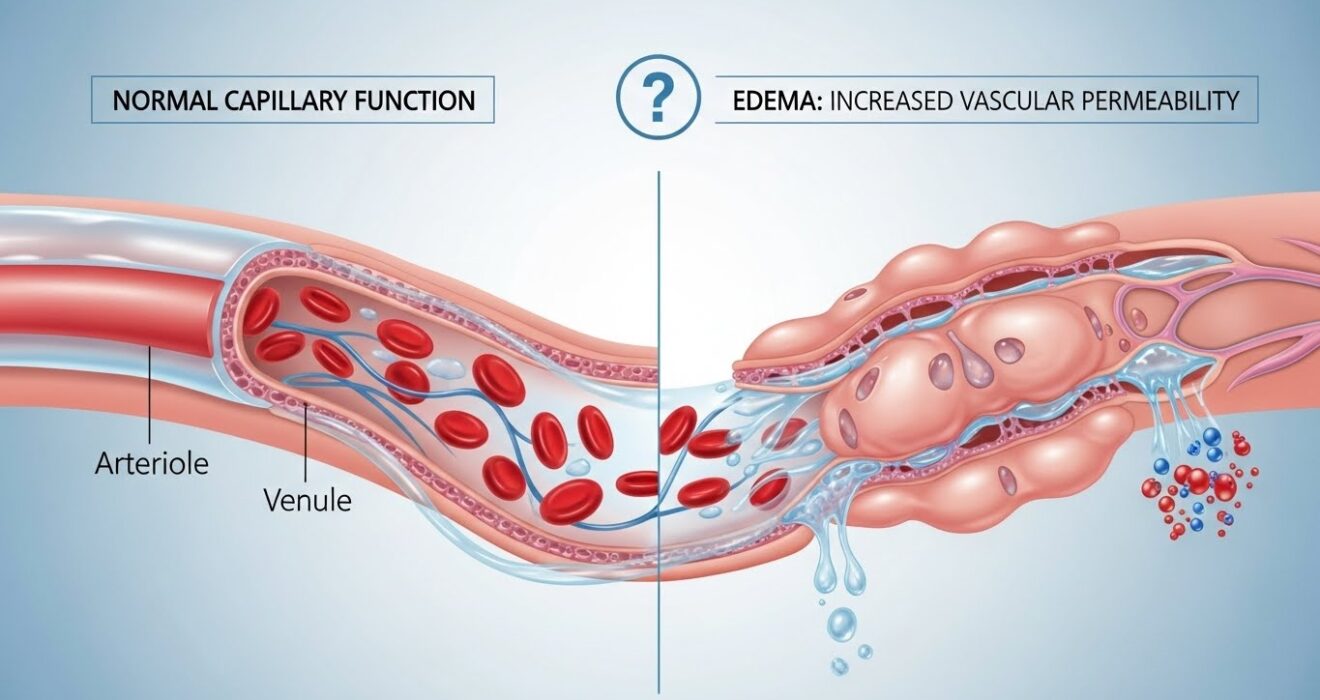
In medical terms, leg swelling is known as edema. It occurs when excess fluid becomes trapped in the body’s tissues. While edema can affect any part of the body, it is most frequently observed in the hands, arms, feet, ankles, and legs.
Edema in legs happens when the small blood vessels leak fluid into nearby tissues. This buildup makes the tissue swell. Identifying the difference between temporary fluid retention legs caused by lifestyle factors and chronic issues is vital. For example, mild lower limb swelling after a salty meal or a hot day usually resolves on its own. However, swelling that persists, affects only one leg, or is accompanied by pain usually requires medical attention.
When Leg Swelling Is Related to a Vascular Condition
Vascular conditions are among the most frequent causes of persistent leg swelling. When the circulatory system struggles to return blood to the heart, fluid pools in the lower extremities. Below are the specific vascular issues that lead to swelling.
Chronic Venous Insufficiency (CVI)
Chronic venous insufficiency occurs when the veins in the legs have trouble sending blood back to the heart. Healthy veins contain tiny valves that open and close to keep blood flowing upward. When you have CVI, these are weak vein valves that fail to close properly.
This failure allows blood to flow backward and pool in the legs, leading to venous insufficiency swelling. Patients often notice that symptoms worsen after standing for long periods and improve when the legs are elevated. Venous edema symptoms may also include aching, cramping, or skin color changes.
Varicose Veins
Varicose veins are perhaps the most visible sign of vascular dysfunction. These are twisted, enlarged veins that usually appear blue or dark purple. While many consider them a cosmetic concern, they are a functional problem that causes varicose veins swelling.
When blood pools in these damaged vessels, it increases pressure within the leg, forcing fluid into the surrounding tissue. This leads to heavy or tired legs and visible vein problems. If left untreated, swollen varicose veins can progress to more severe skin changes or ulceration.
Deep Vein Thrombosis (DVT) – A Medical Emergency
Deep Vein Thrombosis (DVT) is a serious condition that occurs when a blood clot forms in a vein located deep inside your body, usually in the legs. This causes sudden blood clot swelling and can be life-threatening if the clot breaks loose and travels to the lungs.
DVT symptoms are distinct from chronic swelling. Look for one leg swollen suddenly, accompanied by pain, tenderness, and warmth over the affected area. If you experience these signs, seek emergency medical care immediately.
Lymphedema
The lymphatic system is part of the immune system and works alongside the vascular system to drain fluid. Lymphedema swelling legs occurs when lymph vessels are blocked or damaged. Unlike venous edema, which is often soft, lymphedema can cause the skin to feel hard or thick.
Lymph blockage symptoms often start gradually but can lead to significant chronic leg swelling if not managed. This condition requires specialized therapy to encourage fluid drainage.
Peripheral Artery Disease (PAD)
While most vascular swelling is vein-related, arterial issues can also play a role. Peripheral Artery Disease (PAD) is the narrowing of the arteries that carry blood to the limbs. While PAD swelling is less common than venous swelling, poor circulation legs can lead to fluid accumulation when the limb is in a dependent position (hanging down).
Artery narrowing symptoms usually include pain when walking (claudication), numbness, or coolness in the leg rather than just swelling alone.
Post-Thrombotic Syndrome
For patients who have previously suffered from DVT, post-thrombotic swelling is a common long-term complication. The clot can cause permanent vein damage after DVT, scarring the valves and lining of the vein. This results in chronic venous swelling, pain, and skin discoloration that persists long after the initial clot has been treated.
Warning Signs That Swelling Is Vascular-Related
Not all swelling indicates a vein or artery problem. However, specific characteristics strongly suggest a swollen legs vascular cause. Be alert for the following vascular swelling signs:
- Asymmetry: One leg swollen causes are often vascular, such as DVT or physical obstruction, whereas heart or kidney issues typically swell both legs equally.
- Timing: Swelling that is minimal in the morning but worsens throughout the day suggests venous insufficiency.
- Physical Sensation: Swollen legs with pain, heaviness, throbbing, or cramping often point to vein disease.
- Skin Changes: Look for visible veins, reddish-brown skin discoloration, or skin that appears shiny and tight.
- Sudden Onset: Sudden swelling with redness or heat is a medical emergency.
Other Non-Vascular Causes of Swelling
To accurately identify a vascular issue, it helps to rule out medical causes of swelling that originate elsewhere in the body. Understanding the difference between swelling vs vein problems ensures you see the right specialist.
Other edema causes include:
- Heart Failure: The heart is too weak to pump blood efficiently, causing fluid to back up.
- Kidney Disease: Kidneys fail to remove excess fluid and sodium.
- Medication Side Effects: Certain blood pressure medicines, steroids, and pain relievers trigger swelling.
- Pregnancy: Increased fluid volume and pressure from the uterus.
- Injury: Sprains or strains causing localized inflammation.
How Vascular Swelling Is Diagnosed
Accurate diagnosis is the cornerstone of effective treatment. A vascular specialist will begin with a physical exam to check for swelling, discoloration, and pulses.
Advanced diagnostic tools include:
- Vascular Ultrasound: This non-invasive test uses sound waves to visualize blood flow and detect clots or valve failure.
- Venous Doppler Test: A specific type of ultrasound to measure the speed and direction of blood flow.
- ABI Test Legs: The Ankle-Brachial Index compares blood pressure at the ankle to the arm to check for PAD.
Treatment Options for Vascular-Related Leg Swelling
Once diagnosed, the goal is to reduce swelling and prevent complications. The best treatment for leg swelling depends on the severity of the condition.
Lifestyle & Home Care
Conservative management is often the first step. To improve leg circulation and reduce leg swelling naturally:
- Leg Elevation: Keep legs raised above heart level for 15-20 minutes several times a day.
- Movement: Avoid sitting or standing for long hours. Flex ankles frequently.
- Exercise: Walking engages the calf muscle pump, which helps push fluid out of the legs.
- Swelling Home Remedies: A low-salt diet helps prevent overall fluid retention.
Medical Treatments
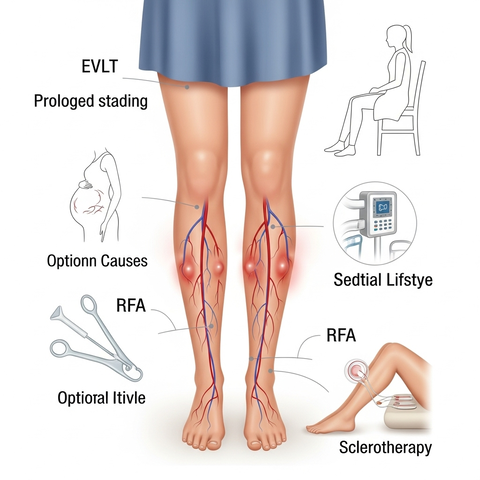
If lifestyle changes are insufficient, medical intervention is necessary. Vascular swelling treatment options include:
- Compression Therapy: Prescription-strength compression stockings squeeze the legs to help veins move blood upward.
- Medication: Anticoagulants (blood thinners) are standard for DVT, while other drugs may treat PAD.
- Vein Treatment Options: Procedures like sclerotherapy (injecting a solution to close veins) effectively treat smaller varicose veins.
When Surgery Is Needed
For advanced disease, minimally invasive vascular surgery or other vascular procedures may be required.
- Endovenous Ablation: Using heat or laser to seal damaged veins.
- Vein Surgery Options: Phlebectomy removes larger surface veins.
- Artery Blockage Treatment: Angioplasty or stenting opens narrowed arteries in PAD patients.
When to See a Vascular Specialist
Timely medical advice prevents irreversible damage. You should search for a “vascular doctor near me” or specialist for swollen legs if:
- Swelling persists for more than a week despite home care.
- You have sudden one-leg swelling.
- You notice leg swelling checkup warning signs like skin ulcers or discoloration.
- You are a diabetic patient experiencing leg changes.
- You need a varicose vein specialist for cosmetic or functional relief.
Prevention Tips for Healthy Veins
Preventative care helps maintain vascular health and prevent leg swelling. Adopting healthy vein habits can improve blood flow legs and reduce the risk of vein disease symptoms.
- Maintain a Healthy Weight: this takes pressure off of your leg veins.
- Stay Active: Regular exercise improves circulation problems in legs.
- Hydration: Drinking water helps flush out excess salt.
- Avoid Prolonged Positions: Take breaks to move around if you work at a desk.
Frequently Asked Questions
Does drinking more water help with leg swelling?
Yes. Dehydration causes the body to hold onto fluids as a survival mechanism. Drinking adequate water helps flush out excess sodium and reduces fluid retention legs.
Is walking good for swollen legs?
Absolutely. Walking activates the calf muscle pump, which is essential for pushing venous blood back toward the heart. It is one of the most effective ways to improve leg circulation.
When is leg swelling an emergency?
Leg swelling is an emergency if it occurs suddenly in one leg, or is accompanied by chest pain, difficulty breathing, or coughing up blood. These are signs of a pulmonary embolism caused by DVT.
Prioritize Your Vascular Health
Leg swelling is often a signal that your circulatory system requires attention. While some causes are temporary, vascular conditions like CVI and DVT require expert medical management. Early diagnosis not only alleviates discomfort but also prevents severe long-term complications.For those seeking the highest standard of diagnosis and treatment, Vascular Care is the best service provider to trust with your circulatory health. Our team specializes in identifying the root cause of leg edema causes and providing tailored solutions. Vascular health equates to overall health; do not wait until symptoms disrupt your daily life to seek the care you deserve.