How Diabetes Affects Your Blood Circulation
Managing diabetes involves more than just monitoring blood sugar levels; it requires a comprehensive understanding of its potential complications. One of the most significant concerns is how diabetes affects blood circulation. Over time, high blood sugar can damage your blood vessels, leading to serious health issues, particularly in your legs and feet.
This guide will explain the connection between diabetes and circulation, outline the warning signs of poor blood flow, and provide actionable steps to protect your vascular health. Early prevention and proactive care are critical to avoiding severe complications and maintaining your quality of life. Understanding these risks is the first step toward effective diabetes management.
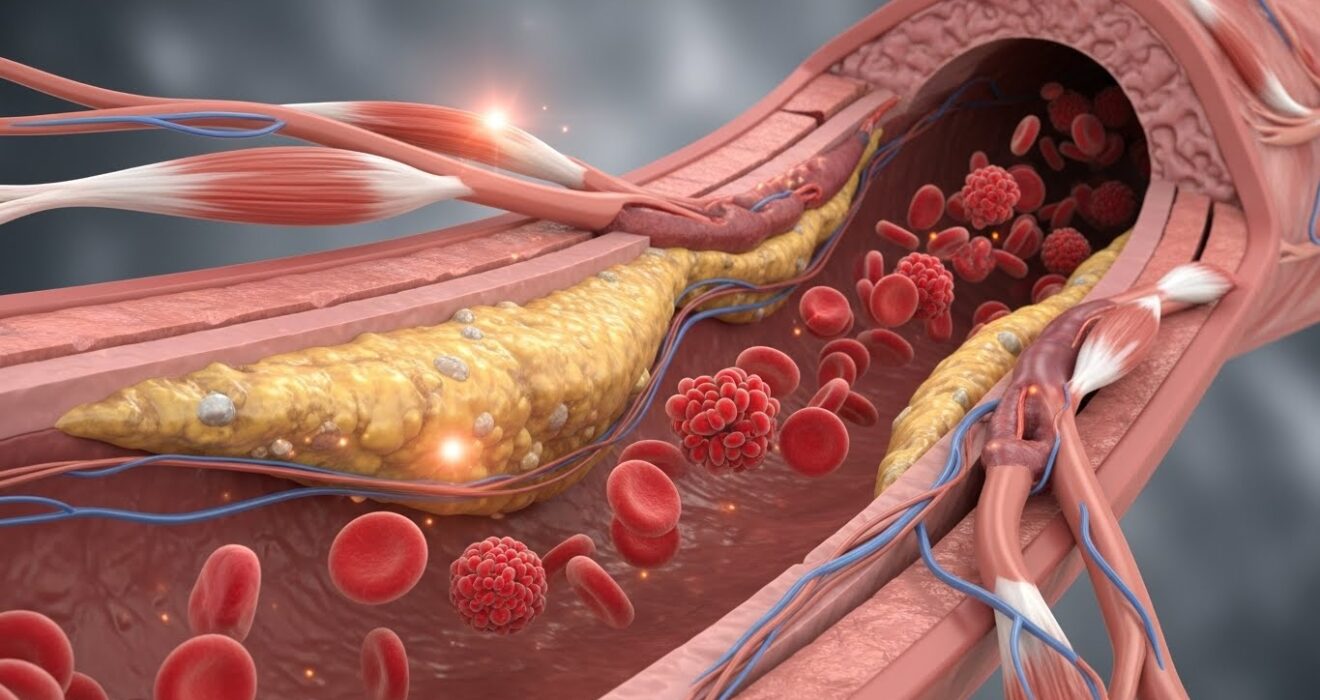
How Diabetes Affects Blood Circulation
The core of diabetes-related circulation problems lies in the effect of high blood sugar (hyperglycemia) on your blood vessels. Consistently elevated glucose levels can damage the inner lining of your arteries, making them less flexible and more susceptible to narrowing.
This process, known as atherosclerosis, involves the buildup of plaque (a mix of fat, cholesterol, and other substances) inside the arteries. As these passages narrow, it becomes more difficult for blood to flow freely throughout your body. Consequently, the delivery of oxygen and essential nutrients to tissues and organs is compromised. This reduced blood flow is the primary cause of many diabetic complications, from slow-healing wounds to severe vascular diseases.
Poor Circulation in Diabetes: What Happens?
When blood flow is restricted, your extremities—especially the legs, feet, and hands—are often the first to show signs of trouble. The reduced supply of oxygen-rich blood means tissues don’t receive what they need to function correctly and repair themselves. This can cause a lot of complications.
Wounds and sores may heal much more slowly than they should, increasing the risk of infection. Furthermore, many people with diabetes also develop nerve damage (diabetic neuropathy), which can cause a loss of sensation. This combination is particularly dangerous; you might not feel a small cut or blister, and poor circulation will prevent it from healing properly, creating a gateway for serious infections.
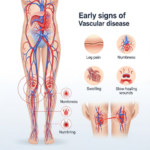
Early Signs of Poor Circulation in Diabetics
Recognizing the early signs of poor circulation is essential for preventing long-term damage. If you have diabetes, pay close attention to the following symptoms.
Numbness or Tingling in Feet and Hands
Numbness or a “pins and needles” feeling is often one of the earliest indicators of peripheral neuropathy. . This condition results from nerve damage caused by high blood sugar and reduced blood flow.
Cold Feet or Hands
If your feet or hands consistently feel cold, even in a warm environment, it may indicate that not enough warm, oxygenated blood is reaching your extremities.
Slow-Healing Cuts or Wounds
A diminished blood supply means less oxygen and fewer nutrients are available for tissue repair. Even minor cuts, blisters, or sores can take an unusually long time to heal, significantly raising the risk of infection and diabetic foot ulcers.
Leg Pain or Cramping While Walking
Pain, cramping, or tiredness in your leg or hip muscles during activity, which subsides with rest, is a classic symptom of peripheral artery disease (PAD). This condition, known as claudication, is caused by narrowed arteries that cannot supply enough blood to your muscles during exertion.
Skin Color or Texture Changes
Poor circulation can alter the appearance of your skin. You might notice that the skin on your feet or legs looks pale, bluish, or shiny. It may also become dry and cracked due to a lack of nutrients, making it more vulnerable to injury.
Swelling in Feet or Ankles
When blood flow is inefficient, fluid can accumulate in your tissues, a condition known as edema. This often causes noticeable swelling in the feet, ankles, and lower legs.
Conditions Caused by Poor Circulation in Diabetics
If left unaddressed, poor circulation can lead to severe and sometimes life-threatening conditions.
- Peripheral Artery Disease (PAD): This is a common and serious complication where plaque buildup narrows the arteries carrying blood to your legs and feet. People with PAD are more likely to have heart attacks and strokes.
- Diabetic Foot Ulcers: A combination of poor circulation and neuropathy can lead to the formation of open sores, or ulcers, on the feet. These non-healing wounds can become deeply infected.
- Infections and Gangrene: Because poor circulation impairs the body’s ability to fight infection, minor wounds can escalate quickly. In severe cases, tissue death (gangrene) may occur, potentially requiring amputation.
- Nerve Damage (Neuropathy): The link between circulation and neuropathy is a vicious cycle. Poor blood flow damages nerves, and damaged nerves can reduce your ability to detect injuries, leading to further complications.
How to Improve Blood Circulation with Diabetes
The best treatment for diabetic circulation issues is proactive management. By taking control of your health, you can significantly improve blood flow and reduce your risk of complications.
1. Control Your Blood Sugar
The most important step is to keep your blood glucose levels within your target range. Regular monitoring and working with your doctor to maintain stable HbA1c levels will prevent further damage to your blood vessels.
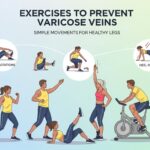
2. Get Regular Exercise
Physical activity is crucial for improving blood flow. Low-impact exercises like walking, cycling, and swimming stimulate circulation. Simple foot exercises, such as pointing and flexing your toes, can also help while you are sitting.
3. Stay Hydrated
Drinking enough water helps maintain optimal blood viscosity, allowing it to flow more easily through your vessels.
4. Quit Smoking
Smoking accelerates the hardening and narrowing of arteries, drastically worsening vascular damage. If you have diabetes, quitting smoking is one of the most effective actions you can take to protect your circulation.
5. Practice Proper Foot Care
Inspect your feet daily for any cuts, blisters, or color changes. Keep them clean, dry, and moisturized to prevent cracking. Trim your toenails carefully to avoid ingrown nails.
6. Wear Compression Stockings (If Recommended)
For some individuals, a doctor may recommend compression stockings to help improve blood flow from the legs back to the heart and reduce swelling.
When to See a Doctor
Do not ignore symptoms of poor circulation. Schedule an appointment with a vascular specialist if you experience any of the following:
- A wound on your foot or leg that is not healing
- Persistent numbness, tingling, or pain in your extremities
- Changes in the color or temperature of your skin
- Pain in your legs when walking
Early diagnosis and intervention are key. A vascular care expert can provide a precise diagnosis and create a treatment plan tailored to your needs. At Vascular Care, our specialists are dedicated to providing the best service and outcomes for patients with diabetic circulation issues.
Take Control of Your Vascular Health
Poor blood circulation is a serious but manageable complication of diabetes. By controlling your blood sugar, adopting a healthy lifestyle, and being vigilant about any new symptoms, you can protect your blood vessels and prevent severe consequences.
Don’t wait for a small problem to become a major one. If you have concerns about your circulation, seek professional medical support. A partnership with a trusted vascular specialist is essential for proactive care and long-term health.
Frequently Asked Questions (FAQs)
1. Why does diabetes affect circulation?
Diabetes can damage blood vessels and the nerves that control them due to consistently high blood sugar levels. Over time, this can lead to restricted blood flow and an increased risk of complications such as peripheral artery disease or even ulcers.
2. What are the warning signs of poor circulation?
Common signs include numbness or tingling in the extremities, cold hands or feet, leg pain while walking, slow-healing wounds, and changes in skin color or texture. If you notice these symptoms, it’s important to consult your healthcare provider promptly.
3. How can I improve my circulation if I have diabetes?
Good blood sugar control, regular physical activity, maintaining a healthy diet, and avoiding smoking are key steps. Additionally, managing cholesterol and blood pressure levels can further protect your vascular health.
4. When should I see a specialist?
If you’re experiencing persistent symptoms of poor circulation or if lifestyle changes and medications aren’t effectively improving your condition, it may be time to consult a vascular specialist. Early intervention is critical to avoiding severe complications.
5. Can poor circulation lead to other complications?
Yes, if left untreated, poor circulation can contribute to serious issues such as infections, ulcers, or even the need for amputations in severe cases. However, with proper management and regular medical care, these risks can be significantly reduced.